söndag 16 februari 2025
Empty Nose Syndrome (ENS) Tragedy: Scott Gaffer's Struggle and Legacy
Empty Nose Syndrome After Nasal Surgery – The Tragic Story of Yaneiv Oz

Näsplastik och reduktion av näsmusslor – John Malamos tragiska öde (1967–2010)
John Malamos, USA 1967-2010. Baserad på Intervju med johns bror
John Malamos bodde i Illinois, USA, och levde ett liv fullt av glädje och energi tills han genomgick två kosmetiska näsoperationer. Därefter tog hans liv en mörk vändning som till slut ledde till hans alltför tidiga död vid endast 43 års ålder. Den första operationen genomfördes utan att han upplevde några märkbara andningsproblem. Tyvärr utfördes ingreppet inte korrekt, vilket gjorde att han var tvungen att genomgå en ny operation. Under denna korrigering valde kirurgen att även reducera hans nedre näsmusslor, utan att informera John om riskerna med detta ingrepp. Denna onödiga reduktion utlöste en rad hälsoproblem, inklusive sömnlöshet, torrhet, smärta, kvävningskänsla, ångest och depression.
Johns bror Thomas delade hans historia som en viktig påminnelse om att noggrant informera sig om alla ingrepp som en kirurg kan utföra och att tydligt kommunicera att man vill undvika onödiga "tilläggsoperationer" såsom reduktion av näsmusslor. John trodde att han endast skulle genomgå en korrigering av sin kosmetiska operation men vaknade upp med både en korrigering och en reducering av sina nedre näsmusslor. Detta ingrepp hade inget att göra med hans kosmetiska operation, och det är nästan säkert att John fortfarande hade varit vid liv idag om kirurgen inte hade utfört denna extra åtgärd, vilket ledde till att han drabbades av den fruktade sjukdomen Empty Nose Syndrome (ENS).
Innan sin operation levde John livet till fullo och hade knappt några bekymmer. Han var en passionerad motorcyklist som älskade att resa till västra USA med sina motorcykelvänner. Han hade en stadig flickvän, en nära vänkrets, familj i närheten och en givande karriär som assisterande chef på Costco. John var en källa till värme och glädje i sitt samhälle – en man vars närvaro kändes djupt av alla runt honom.
Både kollegor och kunder på Costco minns honom med värme. Än idag, över tio år senare, delar de historier om hans vänlighet och exceptionella ledarskapsförmåga när hans bror besöker butiken för att handla. John hade en sällsynt talang för att få alla runt sig att känna sig uppskattade och sedda. De hundratals kollegor som deltog på hans begravning och lämnade kommentarer i hans dödsannons är ett tydligt bevis på den positiva påverkan han hade på så många liv. Nedan är några av de många kommentarer som lämnades av hans kollegor online. (1)
"John var en av de där unika människorna. Den mest medkännande och kära vän och chef. Jag kommer alltid att minnas våra samtal om livet och hur många gånger John hjälpte mig genom svåra tider. Jag kommer att sakna honom djupt."
Kristin Harbke, October 10, 2010
"Jag lärde känna John när jag började på Costco 2002. Han hälsade alltid med ett smittande leende, och vi fick alltid ett gott skratt tillsammans. Han var mer än bara en kollega – John var en fantastisk vän. Det är sällsynt att möta någon så utåtriktad och medkännande som John. Vi höll kontakten genom åren, och jag blev oerhört ledsen när jag fick höra om hans bortgång. Mina tankar och böner är med familjen Malamos under denna svåra tid."
Patrick Hayes, 28 oktober 2010
"Jag skulle inte vara där jag är idag utan John. Han gav mig inte bara möjligheten att arbeta på Costco, utan han gav mig en andra chans i livet och fick mig alltid att le, även under de tuffaste dagarna. Han tog sig alltid tid att fråga hur jag mådde och fick mig att känna mig uppskattad. Jag saknar dig verkligen och tackar dig för allt du har gett mig."
Jeff Wilkalis, 7 augusti 2011
"John, det har gått så lång tid sedan du lämnade oss, men det känns som igår. Vi saknar dig fortfarande så mycket och minns dig genom att dela våra minnen av dig. Livet är inte detsamma sedan du gick bort. Jag saknar hur du alltid tog dig tid att prata med oss och hjälpa till med livets problem. Du var en sådan omtänksam person. Du kommer alltid att leva kvar i mitt hjärta. Hälsa till Audrey – jag vet att hon skulle leta efter dig med öppna armar. Må du fortsätta vila i frid och vara lycklig för alltid. Kärlek, Ruth."
Ruth Reynolds, 10 juli 2023
Ett liv som förkortades av näsplastik och reduktion av näsmusslor
Efter operationen av sina näsmusslor tog Johns tidigare lyckliga och uppfyllda liv en mycket mörk vändning. I sin kamp för att förstå varför han kände sig kvävd och inte kunde sova på flera dygn sökte han hjälp vid välrenommerade institutioner som Cleveland Clinic och Mayo Clinic. Tillsammans med sin far reste han hundratals mil för att få svar, och till slut fick han en diagnos – Empty Nose Syndrome (ENS). Men trots diagnosen hade varken Cleveland Clinic eller Mayo Clinic några behandlingsalternativ att erbjuda eller läkare i hans närhet att hänvisa till. Hans hopp krossades när han insåg att det inte fanns någon lindring att få och att hans livskvalitet skulle förbli mycket låg.
John blev alltmer orolig och djupt deprimerad som en följd av ENS. Detta oroade hans familj, då han inte hade några kända psykiska problem före operationen. Han fick psykiatrisk vård och vistades en tid på en psykiatrisk klinik, men detta gjorde honom bara mer isolerad och hopplös – roten till hans lidande var fysisk, inte psykisk.
I sina mörkaste stunder gjorde John flera försök att avsluta sitt lidande. Han försökte först begå självmord genom att använda kolmonoxid från bilens avgassystem men ångrade sig i sista stund. Ett senare misslyckat försök innefattade en hängning. Till slut stal han en revolver vid ett besök hos en familjemedlem och tog sitt liv dagen därpå. Hans tragiska och alltför tidiga bortgång lämnade familjen i djup sorg.
Det var särskilt betydelsefullt för Johns familj att kunna visa för sin kyrka att hans död var en följd av en svår fysisk sjukdom. Detta möjliggjorde att hans begravning och ceremonier kunde genomföras enligt den grekisk-ortodoxa traditionen.
Thomas Malamos delar nu sin brors historia i hopp om att öka medvetenheten och förhindra framtida tragedier. Han vill att människor ska förstå den allvarliga och onödiga påverkan som ENS kan ha på en människas liv. Thomas är övertygad om att John aldrig skulle ha fått sina näsmusslor reducerade om han hade blivit informerad om riskerna och fått vara delaktig i beslutet.
Liksom många andra vänner och familjemedlemmar som har förlorat sina nära till ENS, frågar sig Thomas varför kirurgen opererade på Johns näsmusslor. Var det för att tjäna mer pengar? Var det för att de inte hade fått tillräcklig utbildning om näsmusslornas betydelse under sin läkarutbildning? Saknade kirurgen den skicklighet och precision som krävdes för att operera resten av näsan utan att röra näsmusslorna? Att få svar på dessa frågor skulle kunna hjälpa andra att undvika samma öde som hans bror.
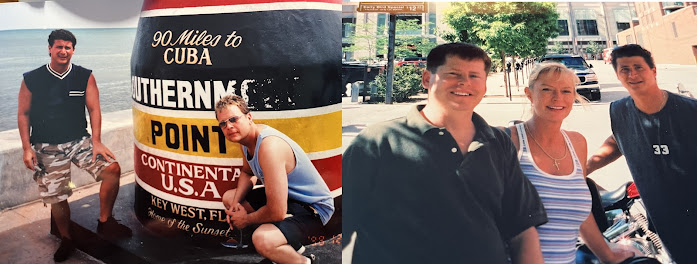
Som en del av att hedra Johns minne har Thomas delat fotografier och videor från lyckligare tider – ögonblick fyllda med skratt, äventyr och glädjen i att leva livet fullt ut. Dessa bilder är en påminnelse om den person John var innan sjukdomen tog över, och speglar ett liv som var ljust och fullt av löften. Det är så Thomas vill att hans bror ska bli ihågkommen av andra.
(1) Kommentarer från vänner och kollegor i dödsanonsen
John Malamos' PDF file kan läsas här (Det tar en kort stund att ladda filen)The Tragic Cost of Medical Neglect: Jack Ackland’s Battle with Empty Nose Syndrome
Jack, a devoted Air Force veteran, served his country with immense personal sacrifice. His struggles began with sinus issues that worsened during flight training. In search of relief, Jack underwent several sinus surgeries over the years. Under pressure from superiors, he also had a turbinectomy performed, a procedure that left him disabled and ultimately ended his military career. Read Jacks PDF file here.
Initially, Jack held onto hope that these surgeries would ease his sinus issues and allow him to continue flying, but the outcome was far from what he had envisioned. Each surgery brought complications and did not ease his pain. Instead, they led to a condition known as Empty Nose Syndrome (ENS). This syndrome occurs when excessive tissue is removed from the nasal passages, leaving the patient with a feeling of nasal obstruction, despite the physical space being open. Jack felt suffocated by the very air that was supposed to relieve him, leading to profound emotional and psychological distress.
The impact of ENS on Jack’s mental health was devastating. He experienced a significant change in personality, becoming withdrawn and depressed. The physical pain he endured was intensified by the emotional toll of feeling trapped in a body that had been butchered. Jack struggled to articulate his suffering to those around him, which only added to his sense of isolation. His family noticed the changes in him—he became irritable and distant, unable to engage with his loved ones. They could only watch as he battled a silent torment, feeling helpless to alleviate his pain.
In the spring of 1961, overwhelmed by his suffering Jack could no longer endure the pain. He left the house with a .22 caliber handgun and never returned. His suicide was not an impulsive act but rather a culmination of years of physical and emotional struggle, as he felt that his condition had robbed him of his dignity and quality of life.Initially, the Department of Veterans Affairs (VA) ruled that Jack’s suicide was not connected to his military service or his chronic disability. However, his wife, determined to secure recognition of Jack’s struggles and the impact of his service, appealed the decision. In her appeal, she emphasized her inability to support their children on her meager salary of $4,040 a year (equivalent to about $34,000 today) and argued that she was not seeking to defraud the government but simply wanted to ensure her children could pursue their education.
After nearly a year of appeals, the VA reversed its initial ruling and acknowledged the severe impact of Jack's chronic pain and subsequent mental health issues. They ultimately granted his widow a monthly Dependency and Indemnity Compensation payment of $122 (approximately $1,000 today). This decision marked a small victory in recognizing the Empty Nose Syndrome that took Jack's life, though it came too late for him.
Read the full article here. The article can also be found in this PDF file
Excerpts from the Article:"In this hospital, I was placed under the care of Major RW Wright, MD, head of the ENT department. I was determined not to undergo surgery on my sinuses, but after considerable pressure, I ultimately consented to a 'submucosal' operation... referring to a submucosal resection that removes the cartilage and bone from the nose."
"Wright hypothesized that a set of tiny nasal bones called 'turbinates' are often infected and could contribute to ear problems. During Jack's first surgery in March 1943, Wright cut nasal cartilage and bone. He then operated on Jack's turbinates, performing a turbinectomy. Not only was too much of the nasal structure removed, leading to a collapse of the nose, but the ends of the turbinates were resected, resulting in excessive airflow due to an enlarged nasal cavity and atrophic rhinitis. Other doctors criticized the surgery... examining him and deeming the operation 'unnecessary.'"
"Majors Wilucki and Neff in Tucson made very complacent remarks about the well-done work on my nose and expressed doubts about my ability to continue flying but said I deserved a chance to try, Jack recalled in his letter from March 1952. Jack did indeed try, and he failed."
"The symptoms were the same as before hospitalization in Santa Ana, and the pain was exacerbated by flying... The symptoms were so severe that he was unable to fly. Jack was grounded, demoted to private with 'no prejudice,' and sent to Amarillo Air Force Base for assignment," he wrote in his 1952 letter.
Len writes: "I now knew the details of his surgery, but I still had a significant unanswered question: why did Wright, an experienced surgeon, perform such a radical operation that left my father too disabled to continue his service? Did he, in the eyes of other doctors, botch the surgery? Were his resections intentional or the mistakes of an overworked military surgeon?"
"While I could not determine Wright's surgical rationale for my father, the results of the operation are indisputable. I asked Dr. Robert M. Meyers, an ENT professor at the University of Illinois in Chicago, to review the details of Jack's surgery and its consequences. Meyers stated that surgical procedures in the 1940s were 'performed coarsely compared to today.' Today, he said, Jack's condition would be referred to as 'Empty Nose Syndrome.'"
"In November 1946, he was hospitalized for sinusitis and streptococcal sore throat... resulting in 'specific arthritic infection and acute rheumatic fever with almost septic temperatures and significant swelling in each joint, to the point that his wife did not recognize him.' Jack wrote, 'It is thanks to the care of Dr. Brenann and his colleagues... that I finally pulled through, and on Christmas Day, my wife was informed that I was expected to live.'"
"After 1946... Jack filed a claim with the VA for an increase in his disability rating, seeking more benefits. He and his civilian doctors argued that the chronic bronchitis caused by the aftereffects of his sinus issues should be considered alongside the disability for sinusitis. The following September, the VA rejected his claim... His unsuccessful appeal to the VA included a supporting letter from Dr. E.R. Fenton of Washington: 'Mr. Ackland came to see me on December 31, 1943, and I have seen him regularly since. He has constant drainage from his posterior sinuses and an acute bronchial cough from bronchial pneumonia and pleurisy. He has been thoroughly examined... and there is nothing we could do to clarify this situation. Following these infections, the patient has suffered from infectious arthritis. In my opinion, the disability is permanent and total. I have recommended his retirement from official duties and that he seek a warm, dry climate in which to live.'"
Jack writes: "It is often necessary for me to lie down immediately after work so that I can show up the next day... However, violent headaches, many sore throats, arthritis attacks, weight loss, general debility, and sensitivity to pneumonia and similar respiratory illnesses are all the result of my disability."
His colleagues write: "He often seemed on the verge of collapsing when he left the office to go home or to the hospital... to be treated. There were times when the pain brought him down, and Mrs. Ackland had to come and drive him home." Jack "was hospitalized again in March 1961. This time, he was placed in isolation, which broke his heart as he felt contagious to his family and friends, leading to significant psychological distress... Jack said he felt 'a burden to his family.'"
"On Father's Day, and my brother's sixth birthday, Dad was too ill to accompany the rest of the family to Elitch Gardens amusement park. The next morning, at dawn, Mom woke me and said, 'Len, Len, your father is gone; he didn’t come home, and he has a gun.' It was a .22 caliber handgun he had purchased a year earlier... I jumped out of bed, quickly dressed, and took the little Pontiac Tempest to look for him. He had taken our second car... I drove north for a few miles to our usual shooting spot. Nothing. Then, on the way back, I spotted the Buick in the line of parked cars... a place where he undoubtedly expected a stranger to find him. Instead, it was me."
"Eleven months after Dad's death, the VA reversed its decision. Based on the evidence of the case, the agency clinically noted that Jack's pain had a psychological impact. They 'determined that there was a definite change in personality with behavioral disturbances and psychiatric manifestations symptomatic of an acquired mental disorder that caused psychological distress. This mental disorder existed at the time of the suicide. This mental disorder was recognized as being directly related to the consequences of sinusitis and bronchitis.'"
This article, written in 2018 by Len Ackland, a journalist and the son of a World War II veteran, recounts the journey and suffering of his father, Jack Ackland, who fell victim to Empty Nose Syndrome. The journalist investigates the causes of his father's suicide, who underwent a turbinectomy performed by the same ENT surgeon in 1943, followed by a Caldwell-Luc operation. Jack Ackland aspired to become a fighter pilot but suffered from barometric sinusitis, leading to frontal pressure, neuralgia, and sinus problems. Under pressure from his superiors, Jack underwent a turbinectomy, a procedure that left him disabled and ultimately ended his military career. Len Ackland describes the ordeal his father courageously endured for 18 years until he took his own life in 1962 at the age of 42. Terms such as "atrophic rhinitis," "empty nose syndrome," "submucosal resection," "removal of nasal cartilage and bone," "turbinectomy," "disability," and "psychological distress" are mentioned. Although his disability was linked to these surgeries, he was repeatedly denied the benefits he was owed. Seventy-five years later, what has changed? Turbinectomies are still being performed today. In April 2020, Marcio Goulart committed suicide following a turbinectomy performed two years earlier, during which the ENT surgeon resected nearly all of his turbinates. Marcio Goulart took his life because he could no longer endure his suffering; he was born on October 9, 1988, and was only 32 years old. On the Empty Nose Syndrome Awareness Forum, on April 26, 2020, Mari Garb wrote: "Hi, I come to inform you that the funeral of our dear friend Marcio is scheduled for 3 PM in the state of Minas Gerais in Brazil. May we bring prayers and a lot of light to him and his family in this sad moment of farewell."
lördag 15 februari 2025
Septoplasty & Turbinate Reduction: A Life Interrupted – Bente Van de Veerdonk’s ENS Story
Instagram Facebook Linkedin Bentes posts in an ENS group This page in word
Empty Nose Syndrome yet a tragic story -Introduction
Bente Van de Veerdonk was a vibrant and determined young woman from Oss, Noord-Brabant, in the Netherlands. Born on December 28, 1997, she had a promising future, skillfully balancing her aspirations in marketing and communication with a career in childcare. Tragically, her life was cut short in November 2024, just 1.5 months shy of her 27th birthday, after a devastating struggle with health issues related to septoplasty and turbinate reduction.
During the septoplasty, Bente's inferior turbinates were reduced using coblation, a method that burns the nasal turbinates. This procedure ultimately led to Empty Nose Syndrome (ENS). Alongside ENS, Bente also battled Crohn's disease and thyroid imbalances, which further compounded her significant health challenges.
A Life of Ambition and Dedication
Bente’s educational journey reflected her passion for learning and personal development. She pursued childcare studies at ROC de Leijgraaf from 2014 to 2017, earning qualifications as a pedagogical employee. Her dedication to children shone through her work at Avem Kinderopvang from July 2019 to November 2021, where she provided care and early childhood education. She later decided to further her education, studying marketing and communications at LOI (Leidse Onderwijsinstellingen) in 2023, aiming to broaden her professional horizons.
A Multifaceted Health Struggle
In addition to her professional and academic pursuits, Bente faced chronic health challenges. She was diagnosed with Crohn’s disease, an inflammatory bowel condition. She also battled thyroid imbalances that left her body in a fragile and unpredictable state. Despite these challenges, she remained hopeful, seeking alternative therapies such as homeopathy and consulting with specialists to find relief.
The Nose Surgery That Changed Everything
In early 2024, Bente underwent nasal surgery to correct a deviated septum and reduce enlarged turbinates. The procedure included septoplasty and bilateral turbinate reduction performed using coblation, a technique often described as low-risk and intended to improve nasal airflow. However, as in many other cases, the surgery led to immediate complications that progressively worsened over time. Her post-operative care involved the use of corticosteroid nasal sprays, which Bente believed further damaged her nasal mucosa.
Brentes symptoms were severe and unrelenting:
Feeling of excessive airflow through the nose.
A persistent burning sensation in her nostrils. The nasal pain was described as severe and unrelenting.
Severe nasal dryness and crusting, worsened by corticosteroid nasal spray prescribed post-surgery.
Slept with her mouth open due to nasal discomfort, which exacerbated dryness.
A sensation of hyperventilation and inability to sense airflow during exhalation. Hyperventilation was worst at night.
Sleep deprivation, including periods of up to five days without rest.
Constant awareness of breathing, leading to severe hyperfocus on it.
Difficulty focusing on everyday tasks, as even watching television became unbearable.
Systemic effects such as dry eyes, a lump in her throat, painful ears, and burning sensations in her chest and limbs.
These symptoms pointed to Empty Nose Syndrome (ENS), a condition where the nasal passages feel overly open, disrupting normal breathing and airflow sensation.
Experimented unsuccessfully with nose clips, tape, and other methods to block excessive airflow.
Other Symptoms Likely Related to ENS:
Dry eyes and mouth.
Difficulty swallowing and a persistent feeling of a lump in her throat.
Ear pain.
Burning sensations across her chest, arms, and back.
Other Medical Conditions:
Reported her thyroid was "close to being too hard," indicating hyperthyroidism or another form of thyroid dysfunction.
A Desperate Search for Relief
Bente sought help tirelessly, consulting with specialists, including plans to visit Dr. Dixon, an ENS expert in Rotterdam. She explored treatments ranging from nasal ointments and warm beverages to alternative therapies like homeopathy. Despite her efforts, the relief was fleeting or nonexistent. On online forums, she vulnerably shared her experiences and sought advice, expressing both hope and despair.
In one poignant post, she wrote:
"I can’t focus on anything else but my breathing. Sleeping is a BIG issue... I really need help to make it a bit more bearable because now I can’t even focus on the TV. You have to imagine."
Her desperation was palpable as she detailed her struggles with insomnia, dependence on lorazepam, and her declining mental health. She expressed fear, isolation, and a longing for a solution that never came.
Bente Van de Veerdonk - The Final Days
In the ten months following her surgery, Bente’s quality of life deteriorated drastically. Once manageable, her health challenges became insurmountable. By the time of her death in november 2024, she had endured sleepless nights, chronic pain, and the emotional toll of feeling her body "failing in every way." Despite her relentless search for hope and support, her suffering became too great to bear and she ended it herself.

A Legacy of Awareness
Tragically, Bente became the sixth individual in 2024 to take her own life as a result of the unrelenting suffering caused by Empty Nose Syndrome (ENS).
Earlier this year, others suffering from ENS also took their own lives, including Charly Audes (France), Tyler Kuckelman (US), Océane Flavigny (France), Sam Treffry (Australia, 2024), and a 54-year-old Canadian man (name withheld).
Please note that these names are based on reports from three online ENS support groups on Facebook, with approximately 5,000 to 6,000 members. It is important to emphasize that this number does not reflect global statistics, as the actual number of ENS-related deaths worldwide is likely much higher.
Bente's death was a direct consequence of complications from a septum and turbinate surgery performed by her surgeon. How many more lives must be lost before authorities intervene? When will these dangerous procedures be banned, and when will the medical community be held accountable for the harm they cause?